What is an Acute Care Surgeon and why do we need them?
University Trauma Rounds at St. Michael's Hospital

C. William Schwab
|
More than 113 million Americans visit emergency departments every year - 40 million
for injuries, 4 to 5 million for abdominal problems. This amounts to 6 to 9 million
emergency patients who need prompt evaluation and treatment by a surgeon. A rising
shortage in the surgical workforce is creating a crisis in emergency care. Few broad
based general surgeons are being prepared to take the place of those trained in
the 50's, 60's and 70's. Surgeons today have a narrower spectrum of practice; many
general surgeons limit their scope to several selected operations. Specialist surgeons
are not comfortable taking ER calls. 70-80 million "baby-boomers" are set to retire
in the US in the next 15 years; thousands of boomer surgeons will retire as well,
leaving huge holes in emergency coverage.
Bill Schwab, our trauma rounds lecturer, leads trauma, acute care surgery and surgical
critical care at the University of Pennsylvania. Penn was the first medical school
and university hospital in the United States, founded by Benjamin Franklin. From
2003-2006 Bill served on an Institute of Medicine Task Force on the Crises in Emergency
Care in the US. (Future of Emergency Care Dissemination Workshop Summaries. Megan
McHugh and Peter Slavin, Rapporteurs. The Future of Emergency Care Workshop Planning
Group Board on Health Care Services, The National Academies Press, Washington, D.C.
One of the solutions the task force examined is a new specialty called Acute Care
Surgery, a term coined by American College of Surgeons Board of Regents Chairman
L.D. Britt to describe a system that combines trauma surgery, intensive care and
burn care with expertise in all surgical emergencies. The latter includes treatment
of perforated viscus, sepsis, soft tissue infections, and some thoracic and vascular
surgery. (Britt LD. Acute care surgery: A proposed training curriculum. Surgery
2007; 141:304-6.) These 24/7 emergency surgeons would provide in-house coverage
rather than consultation from home, creating greater efficiencies.
At the University of Pennsylvania, where 30% of admissions are for gunshot wounds,
Bill and his team now have close to ten years experience with an Acute Care Surgery
model of delivering emergency surgical services. Where these models have been initiated
they have been shown to work well. They produce better outcomes, are more efficient,
and they create a life style that is attractive to surgeons. Currently about 70%
of Level I Trauma Centers in the US have in-house surgeons and 60% of these surgeons
are doing emergency general surgery.
In answer to video conference questions, Bill told us his hospital does not have
a dedicated trauma critical care unit, but uses trauma patient protocols within
all surgical ICUs. In response to Richard Reznick's question about the role of alternative
critical care givers, Bill explained they employ nurse practitioners trained in
trauma and critical care medicine. Some centres use Physicians' Assistants, and
more of these advance practice care givers will be needed as work hours decrease
for residents. He feels Advanced Practice Nurses in the SICU are a tremendous asset,
providing continuity and expertise.
|
Redefining the Future of Trauma Surgery as a Comprehensive Trauma and Emergency General Surgery Service
Patrick K Kim, MD, G Paul Dabrowski, MD, FACS, Patrick M Reilly, MD, FACS, Susan Auerbach, MHA, RHIA, Donald R Kauder, MD, FACS, C William Schwab, MD, FACS
JACS 2004
|
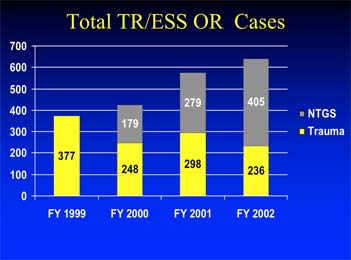
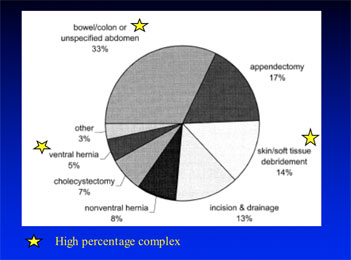
TR = Trauma
ESS = Emergency Surgical Service
Ntgs = Non Trauma General Surgery
|
Some centres use Physicians' Assistants, and more of these advance practice care
givers will be needed as work hours decrease for residents. He feels Advanced Practice
Nurses in the SICU are a tremendous asset, providing continuity and expertise.
Bill went to school in Syracuse, New York and finished surgical training in the
70s. During the Vietnam era he was trained by the US Navy to do "all life and limb
saving surgery". Bill trains surgeons for military service in a special fellowship
program that includes training in emergency craniotomy, especially if that surgeon
might deploy outside the US.
Bibliography:
- Kim PK, Dabrowski GP, Reilly PM, Auerbach S, Kauder DR, Schwab
CW. Redefining a future of trauma surgery as a comprehensive trauma/emergency general
surgery service. Journal of the American College of Surgeons 199(1):96-101, July
2004.
- Gracias VH, Sicoutris CP, Stawicki SP, Meredith DM, Horan AD, Gupta
R, Haut ER, Auerbach S, Sonnad S, Hanson CW 3rd, Schwab CW. Critical Care Nurse
Practitioners Improve Compliance With Clinical Practice Guidelines in "Semiclosed"
Surgical Intensive Care Unit. J Nurs Care Qual. 2008 May 29.
M.M
|