Two Important
Advances in Treatment
of Respiratory Failure
1. LUNG TRANSPLANTATION

Marcelo Cypel
|
Because Canada has a low
rate of organ donation, and
because 80% of the 200
lungs that are offered by
donors each year are unsuitable
for transplantation, the
waiting list is continuing to
lengthen. There are currently
80-100 patients on the waiting
list, and 20-30 waiting
patients die each year. As
the population ages, more
and more patients are being listed. "The challenge is not
only how to increase the supply, but also how to keep the
waiting patients alive, using artificial lung technology."
Marcelo Cypel is attacking both problems.
Marcelo is Assistant Professor of Surgery in the Division
of Thoracic Surgery and a Scientist in the Toronto
General Research Institute (http://www.surgicalspotlight. ca/Article.aspx?ver=Fall_2011&f=NewStaff ). His
wife Tatiana is a plastic surgeon who completed a
Master’s Degree and a fellowship at the Hospital for
Sick Children with Chris Forrest. Their 14 month old
daughter is Rafaela. Marcelo is an enthusiastic athlete.
He tries to run 3-4 times per week and plays soccer when
time allows.
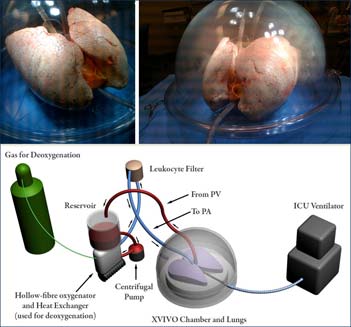 Ex vivo system
|
His outstanding work with Shaf Keshavjee on ex-vivo
perfusion is rehabilitating lungs that are judged to be
unsuitable by conventional criteria. Lungs are shipped
to Toronto to be treated in the ex-vivo system (See figure
1). "We try to protect and preserve the lung, using
normothermic perfusion, gene transfection, antibiotics,
and anti-inflammatory agents to allow the lung to begin
to repair itself. The ex-vivo perfusion circuit is particularly
effective in reversing neurogenic pulmonary edema.
It allows the lung to dry out and for repair of the cell
tight junctions as extra-vascular water is removed." This
work has earned Marcelo multiple honours as a trainee
for basic science papers, oral presentations, including
the McMurrich Award and the Zane Cohen Clinical
Fellowship Achievement Award.
|
"An important area for rehabilitation of the lung is
control of infection. We can clean them up, as the antibiotics
have a long half life. There is no liver or kidney
in the circuit to remove the antibiotics. Nevertheless,
the inflammatory cells and consolidation persist as
an ongoing research challenge. An effective source of
rehabilitated lungs is the organs that are assessed at a
distant site as suboptimal (e.g. because of infection or
poor oxygenation). In the past, we would say we should
not subject our recipients to lungs of questionable quality.
Currently, we are reassessing these lungs, so they are
brought in for perfusion. If 4-6 hours of good function
can be demonstrated on the circuit, the lungs are used."
"Donation after cardiac death (DCD) now accounts for
25% of lung transplants. This number has been increasing
5-10% each year. 90% of centers don’t use the DCD
lungs, but the Toronto group has successfully adopted
this approach. The ex-vivo perfusion system has provided
an objective way to assess these organs and today
DCD lung transplantation is routine at our centre. DCD
is generally accepted in North America; however, only
2% of those end up donating lungs in the United States,
whereas in Toronto at least 30% of DCD lungs are used
for transplantation.
2. PROLONG THE LIFE OF PATIENTS ON THE WAITING LIST WITH ARTIFICIAL LUNGS
"The use of the Novalung as a
bridge to transplant triggered Toronto General Hospital
interest in further developing an Extracorporeal Lung
Support Program (ECLSP). Advances in equipment and
technique have contributed significantly to its usefulness.
For example, avoiding cannulation of the femoral vessels
allows the patients to be mobilized, reducing deconditioning
and associated morbidity. The single cannula double
lumen veno- venous Avalon light system can be used as a
bridge to transplant or as a rescue method for overwhelming
ARDS. Approximately 20 ARDS patients are rescued
by this technique each year. The double lumen cannula can
be inserted in the intensive care unit under fluoroscopy.
The cannula is introduced through the jugular vein. Venous
blood is returned to the oxygenator from the superior and
inferior vena cava, with outflow to the patient from the
second lumen, just above the tricuspid valve. Patients can
be mobilized, eat, converse and avoid the deconditioning
that has been the bane of patients with respiratory failure.
In the past, patients who were dependent on the ventilator
prior to transplantation often required several months of
further ventilation after transplantation - not because of
lung failure, but because of deconditioning. The membrane
oxygenators used are more commonly the Quadrox and
sometimes the Novalung. Neither requires high levels of
anticoagulation."
The ECLS team is organized in three units that report
to Shaf Keshavjee: Surgery- directed by Marcelo Cypel;
Intensive Care by Eddy Fan; and Perfusion by Cyril Serrick.
"The clear well - defined and coordinated protocols and
systems of management rest the lung and eliminate idiosyncratic
management. The ECLS program includes 36 professionals,
surgeons, intensivists and perfusionists. "We are
now much better prepared (better equipment, well trained
staff, protocolized treatment) in the event of future H1N1
type endemic crisis. It is also important for other hospitals
to become aware of this program, as their patients with pulmonary
failure can be referred, not just for transplantation,
but for salvage using the ECLS system."
M.M.
|