A Surgical Ethics Course, and A Sad Footnote on the VA

Martin McKneally
|
The Surgery Department organized
a one day intensive Surgical
Ethics course this spring at the
Toronto Convention Centre. It
was co-sponsored and managed
with the American Association
for Thoracic Surgery at its annual
meeting. The course used the
Teach the Teachers technique
that has worked well for teaching
bioethics to residents at the
University of Toronto for the past 15 years. Instead of
importing ethics scholars, we helped expert surgical
teachers prepare short talks about ethical issues in their
field of specialization.
Cardiac surgeon Vivek Rao discussed the ethics of
rationing mechanical support for failing hearts. “There
is a natural limit on the supply of transplants, but
only an economic limit on the availability of manufactured
LVADs.” Nurse Practitioner-ethicist Jane MacIver
explained the ethics of surgical decision making, based on
her studies of how patients make choices between transplants
and LVADs for advanced heart failure. Surgeonethicist
Karen Devon challenged caregivers to become
involved in the electronic and social media that are
becoming a major source of patient information and disinformation.
Karen described how former Playboy bunny
Jenny McCarthy continues to lead her internet followers
to oppose vaccination, based on the disproven myth of a
link to autism. Her campaign has resulted in outbreaks
of measles, whooping cough and mumps where these
diseases had disappeared. Karen challenged us to engage
and improve the media by refuting false claims.
Cardiac resident Bobby Yanagawa clarified the evolving
and contentious issue of organ donation after cardiac
death. “The dignitary rights of dying donors and their
families are as important as the legal and neurophysiologic
data about the hands-off period. The definition
of death is socially constructed and somewhat variable.”
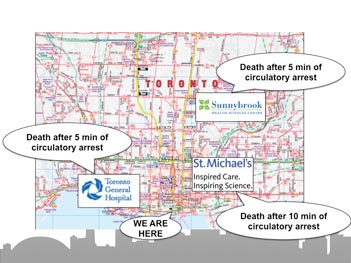
Donation after Cardiac Death criteria vary.
Harvard thoracic surgeon and Chair of the Society of
Thoracic Surgeons Ethics Committee Richard Whyte presented
“Explaining our mistakes to patients”, coached by
our senior surgeon-ethicist Mark Bernstein who was away
during the course. Your editor presented our study of preoperative
discussions of life sustaining treatment (describedin Spotlight Fall 2013).
Surgeons from Syracuse, Wake Forest, Duke, Ohio State,
Cleveland Clinic, Nicaragua, Medical University of South
Carolina, Baylor, and Calgary spoke on topics ranging
from “When is the resident competent to operate independently”
to the “ethics of the learning curve” and “managing
the declining competence of aging surgeons”. Our
Department will offer another Surgical Ethics Intensive
Course next spring.
Course co-director and Medical University of South
Carolina cardiac surgeon Bob Sade recently made my
day by sending references to two publications championing
the fist bump as a safer form of greeting than the
handshake (1, 2). I’ll write more about this in the next
issue, and give a friendly bump to all who have doubted
the wisdom of switching to this cool and safer greeting.
I asked Ken Kizer, our Bigelow Lecturer, whose management
transformed the VA health care system, for
a comment on the disturbing current headlines about
waiting lists, suffering, and deaths of neglected military
veterans in the US. Ken has been out of the VAHS
for the past 15 years. His description of the current
situation is printed nearby. In my view, his remarkable
contributions have been undermined by imposition of
a command and control regime. Militarizing a health
care system under former generals, setting unrealizable
standards with inadequate resources, and reluctance to
accept unfavorable information inevitably led to falsifying
waiting list reports without attending to waiting
patients. There is an excellent Perspective commentary
by Kizer & Jha in the June 4, 2014, NEJM that has
relevant lessons for all health care systems (3).
|
Finally, after 10 years as editor of the Spotlight, I am
searching for an associate editor to work with and then
succeed me. I can promise a stimulating experience -
interviewing the fascinating people who are guests and
members of our surgical family, and learning more than
you ever could imagine about the Department that
binds us together. Writing about all this is illuminating,
because writing requires a level of reflection and justification
that exceeds the requirements of conversational discourse.
This can sometimes be frustrating
but is immeasurably rewarding.
M.M.
1. Sklansky M et al. Banning the handshake from the health care
setting. JAMA online May 15, 2014.
2. Ghareeb PA et al. Reducing pathogen transmission in a hospital
setting: Handshake versus fist bump – a pilot study. J Hosp
Infect. 2013;85(4):321-323.
3. Kizer & Jha, Restoring trust in VA health care. NEJM.org
June 4, 2014.
KEN KIZER ON RECENT PROBLEMS OF THE VA HEALTHCARE SYSTEM
“The recent allegations that some VA medical centers
may have falsified wait time lists to cover up
treatment delays for veterans are deeply disturbing.
Multiple investigations are underway to determine
the validity of the allegations and the extent to
which any veterans may have been harmed. It will
be some time before the findings of these investigations
are known, but I am certain that they will
find that the genesis of the organizational malfunction
in this case is multidimensional. Skyrocketing
demand for services, and especially mental health
service, for veterans returning from the wars in
Iraq and Afghanistan is certainly a factor. Shortages
of some types of health care workers, insufficient
funding or budget flexibility, information technology
and staff training shortcomings, and possible
bad behavior of some administrators also are likely
to emerge as contributing factors.
“However, the fact that more than 20 VA
medical centers are under investigation for possible
improper behavior on the same issue speaks to
deeper, more systemic problems. VA leadership has
turned over multiple times in the past decade with,
unfortunately, a gradual return to the command
and control style of management that predominated
prior to the organization’s transformation in
the late 1990s.
“Concomitant with the changes of leadership
has been successive erosion of the principles of
quality improvement that were integral to the
VA’s turnaround. Hospital managers and clinicians
have been less engaged in the development
of policies and programs that they would have to
implement, and the environment has become less
open, or safe, for them to express criticism or dissenting
views about the directives. Likewise, while
many of the same performance improvement tools,
and especially performance measurement, have
continued to be employed, these tools are now
being used in an increasingly compliance-focused
(instead of improvement-focused) environment.
These dynamics have been further complicated by
the implementation of a pay-for-performance-like
incentive program that ties personal financial gain
to performance measure results.
“Additionally, it has been known for several years
that the information technology and other infrastructure
being used to monitor and track patient
wait times is inadequate for what it is being used for,
although it appears that little has been done to fix the
problems. Given all these circumstances, when VA’s
leadership changed the wait times performance measure
standard from 30 days to 14 days a couple years
ago, it became, in essence, a prescription for driving
administrators to find workarounds. Predictably, not
all of the workarounds would be acceptable.
“On a more positive note, the VA’s current wait
times problems are fixable, and there are thousands
of hardworking, dedicated VA staff who are anxious
to fix them so they can get on with providing high
quality care to veterans.”
Ken Kizer
|
|