Advancing Trauma Care

from left to right: Avery Nathens, Russell Gruen, and Sandro Rizoli
Russell Gruen, Director of the National Trauma Research
Institute and Professor of Surgery and Public Health
at the Alfred and Monash University, in Melbourne,
Australia presented University Trauma Rounds on
Friday, June 7th.
Russell is a general and trauma surgeon with a keen
interest in public health. When he was still in training
in General Surgery at the University of Melbourne,
he completed a PhD on the effectiveness of specialist
outreach clinics for remote indigenous communities in
Northern Australia. He received a Harkness Fellowship
in Healthcare Policy, during which he focused on international
health policy, healthcare systems research, and
medical professionalism. The fellowship took him to
Harvard University where he was also a Fellow in the
medical ethics program. He helped to formulate the
American College of Surgeon’s code of professional conduct.
Russ received his trauma training at Harborview
Hospital in Seattle, where he studied under Avery
Nathens, as the Fellowship Program Director. Russ told
us that Melbourne is similar to Toronto in population,
and in having two major trauma centers. He demonstrated
the effect of various legislative interventions
on reducing the mortality from vehicular trauma (Fig.
1). In recent years, much of this progress is due to the
Victorian State Trauma System.
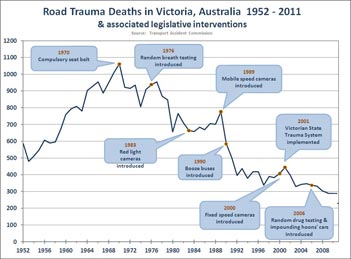
Figure 1
|
He then discussed the perioperative management of
the anti-coagulated patient. Patients taking Warfarin
are commonly encountered in surgical practice, and the
management of their anti-coagulation during surgery
can be suboptimal. In his study of 108 hernia patients
at his own hospital, 30% of those who were “bridged
with low-molecular weight heparin” had significant
bleeding events in the postoperative interval. Bridging
as currently practiced with low molecular weight heparin
is clearly problematical. Many surgeons, particularly
vascular surgeons, now operate without interrupting
anticoagulation. Alternative protocols for Warfarin
reversal, using Vitamin K, or Prothrombinex, also exist,
and there is a need now to evaluate the safety and efficacy
of these in comparison to current guidelines that
use LMWH.
The protocol that he recommends includes vitamin
K, given the night before to get the INR to 1.5. He
presented an excellent summary of the coagulation and
fibrinolysis mechanisms, and the pro-coagulants - hemostatic
adjuncts for the surgeon in current use, including
the recently introduced topical dressings which deliver
thrombin and fibrinogen to the site of bleeding. Newer
preparations include the fibrin pad which can locally
control a 4 mm hole in the aorta in animal models. He
discussed the coagulopathy induced by the combination
of trauma, acidosis, and hypothermia, and the interaction
with the fibrinolytic mechanism. Systemic treatment
for trauma-induced coagulopathy includes fresh
frozen plasma, cryoprecipitate, fibrinogen, Prothrombin
Complex, factor 7A and antifibrinolytics like Tranexamic
acid, and aminocaproic acid.
“In the Crash 2 study of 20,000 patients (www.thelancet.
com/crash-2), tranexamic acid reduced bleeding
deaths in a multi-country study. From our perspective,
the study was limited in that only 2% of the patients
came from countries with advanced trauma care that
included treatments for coagulopathy with blood
products, rapid control of bleeding, and advanced
prehospital and critical care. The remainder came from
countries with less well developed systems, most of
which didn’t have advanced prehospital care and or a
reliable blood supply. Given that the mortality rate of
severely injured patients in Toronto is about half that
of the centres in CRASH-2, it is unlikely that significant
mortality benefit will be achieved in Toronto with
tranexamic acid. The high incidence of bleeding in both
arms of the study probably account for the observation
that tranexamic acid reduced bleeding deaths. From
an observational study in the military, we learned that
tranexamic acid was associated with much higher (9 to
12 times) the incidence of pulmonary embolism and
deep venous thrombosis compared to control patients.
Therefore, there is a need to investigate effectiveness
and safety concerns in advanced systems, such as the
Toronto trauma system.” The PATCH-Trauma trial is
planned to evaluate the pre- hospital administration of
tranexamic acid vs. placebo at the scene of injury in
similar systems.
M.M.
|