Robert Stone Lecture
RETHINKING RESIDENCY TRAINING

Shaf Keshavjee, Bob Stone and Lee Swanstrom
Lee Swanstrom, Professor of Surgery at Oregon Health
Sciences University and Director of the Minimally
Invasive Surgery program, presented the Robert Stone
lecture “Rethinking Residency Training. Perspectives
gained from the Minimally Invasive Surgery Revolution”
at Toronto Western Hospital on Friday, May 13th 2011.
“The laparoscopic revolution began in the late 1980s
when Erich Muhe in Germany did the first laparoscopic
cholecystectomy. He performed 38 operations with one
death. He was reviled by his colleagues, lost his privileges,
was jailed and his wife left him, illustrating the dangers of
being the first. Eddie Joe Reddick brought the technique
of laparoscopic cholecystectomy back from France and
developed weekend courses for general surgeons in North
America. He charged $3,000 for each surgeon to come and
watch him perform the operation. He was able to retire
after five years, then bought a music publishing company.
Eventually, he lost all of his money and went back to work.
He was a better surgeon than he was a businessman.”
The standard approach to surgical residency training
is the Halsted apprenticeship model. Over a period
of 5 to 8 years, surgeons gradually take on increasing
responsibility. They are punished for their mistakes by
withholding progressive opportunities to operate as part
of this training paradigm. Under the old system, training
was long and the pace of surgical evolution was slow. For
example, it took 25 years of operating to achieve the first
survivor of esophagectomy.
Of all the radical revisions introduced by laparoscopic
surgery, weekend courses were the dominant new feature.
These introduced industry participation and marketing
as well as a short duration of training. Laparoscopic
cholecystectomy training had to be rapidly introduced,
so that all 20,000 general surgeons in the United States
could quickly learn the technique. This stimulated
innovation, the rapid development of new instruments,
and rapid introduction of new techniques into practice.
Surgeons who performed laparoscopic surgery could
control their own practice. Hospitals advertised the skills
of their laparoscopic surgeons to increase their market
share. By 2005, not only cholecystectomy, but nearly
every operation in the surgical armamentarium had been
done using minimally invasive surgical techniques.
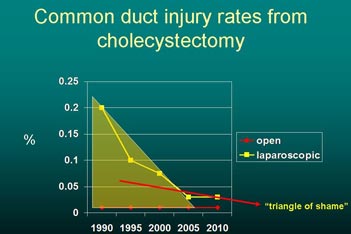
Fig. 1 The Triangle of shame
As it turned out, weekend courses were a mixed blessing,
because training for a weekend left the participants
with no muscle memory and no way for their teachers
to measure their competency. Common duct injuries
were common in the early learning phase of laparoscopic
cholecystectomy, occurring in 0.3% of cases - ten times
the rate of injury in open procedures. This period Lee
refers to as ‘the triangle of shame’. Laparoscopic surgery
proved to be bad for residency training, as teachers were
slow to pass their techniques on. It drove up costs and
introduced conflicts of interest with industry that verged
on the unethical.
|
It is now unacceptable to subject patients to such
learning curves. It stresses the surgeon, the operating
room staff, the healthcare system, and the patients.
With the publication of the IOM’s “To Err is Human”
mandatory improvement in learning new surgical techniques
was required. Current negative influences on the
development of laparoscopic surgery include its cost and
restrictions from the IRB. The reaction to this pushback
has been the development of centers of excellence, where
high volume is equated with expertise. The catch 22 of
this linkage is that it is difficult to get these high volumes
unless you practice in a center of excellence.

Bob Stone, Steve Gallinger and Hugh Scully
One possible solution to the problem is the NICE
Program (National Institute for Clinical Excellence)
introduced in the United Kingdom. The NHS, based
on a NICE evidence review, has decided not to pay for
open colectomy after 2014. In order to ensure that surgeons
become proficient at laparoscopic colectomy, the
government funds regional training centers and pays for
surgeons to attend courses. The government also hired
15 travelling expert surgeons to certify the competence
of those trained at the centres. They visit the surgeons in
the operating room, and proctor their performance. The
American College of Surgeons has also initiated a program
of regional training centers for surgery, but without
the mandate, funding or government backing of the
British system. We also have few measures of competency.
At this time, the American Board of Surgery requires
applicants to have FLS Certification (Fundamentals of
Laparoscopic Surgery) and there will soon be a similar
program for flexible endoscopy (FES). This is timely as
the American Gastroenterological Association and other
medical societies have taken a position that “surgeons are
poor practitioners of gastrointestinal endoscopy and we
shouldn’t be responsible for their training”. The burden
of adequate training and now guaranteeing to the public
that their surgeon is competent clearly rests on the
shoulders of the surgical community.
Short courses don’t work well for residents, and the
reduction in workweek hours has led to a situation where
“training is overreaching and underachieving in general
surgery”. The number of advanced laparoscopic surgical
cases seen in most residencies is usually low. For this reason,
minimally invasive surgery fellowships are needed,
plus the use of virtual reality and internet programs.
Will the system tolerate training as we knew it? How
will we accomplish the “10,000 hours of deliberate
practice?” demonstrated by Ericsson to be necessary for
expert performance. Lee proposes that we change our
thinking about residency training. “We should start at
the other end of the spectrum, introducing residents to
laparoscopic surgery at the beginning, rather than open
techniques. Over time, they can progress to performing
open operations in the 4th and 5th year.” Lee also proposes
that we proctor those who attend short courses,
design ways to measure their competence and train them
toward expertise. During the question period the appropriateness
of screening applicants for three dimensional
spatial sense was raised. Dimitri Anastakis pointed out
that studies completed here and published in the Lancet
show that it is not necessary to exclude applicants whose
three dimensional sense is less developed. They can eventually
be trained to perform at a competent level. Hugh
Scully asked if we are training enough general surgeons
to manage highway crash victims. Lee felt that the direction
that this is going is toward training trauma surgeons
and acute care surgeons, and the use of trauma centres.
Dimitri Anastakis asked how to pay for the $110,000
simulators needed for training. Lee answered that the
US Congress has been asked to address this as it should
be the responsibility of society. Shaf Keshavjee suggested
that industry should pay for the simulator in order to
prepare surgeons to use their $2.3 million devices later
on in their careers. Chris Feindel raised the question of
the effect of limited work hours. “We no longer train
the general surgeon as a universal genius capable of every
operation. The answer seems to be in specialization. ”
M.M with notes from Lee Swanstrom
|