Enhancing Surgical
Performance Using
Simulation
THE GEORGE ARMSTRONG PETERS PRIZE
The George Armstrong Peters Prize celebrates the memory
of Dr. Peters who was described by William Gallie
as "the best technical surgeon of all of my teachers".
The Peters prize is awarded to a young investigator who
has shown outstanding productivity during their initial
period as an independent investigator, as evidenced by
research publications in peer reviewed journals, grants
held, and students trained. In his Peters Prize Lecture,
Teodor Grantcharov, this year's winner, told us that "the
operating room is a high risk environment in which
patients encounter major complications in 3-17% of
cases. Between 44,000 and 98,000 patients in the
United States die because of medical errors. 40% of these
are operating room errors, of which 50% are avoidable."
"The current pressures on surgical education require a
revision in our thinking and training. The hours are shorter
for training, there are decreased clinical opportunities for
residents compared to their teachers, the technology has
become more complex, there is a focus on error, patients
are demanding, and there is a focus on quality of life for
residents. All of these pressures diminish the opportunities
for trainees. Currently, we still hold to the idea that time
is the constant and proficiency is the variable. We still use
subjective assessment, learning by doing, and there has been
little change in the curricula over the last several decades. It
is time for us to move from a fixed time to proficiency as the
criterion for completion
of training."
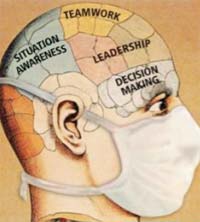
Figure 1
|
Teodor's first
research project
in Toronto asked
the question: Can
simulation training
produce skills
that transfer to the
operating room?
The study results
clearly confirmed
the effectiveness of
simulation training in shortening the learning curves
for surgical trainees. The simulation-trained residents
achieved proficiency before they entered the operating
room. When the cost of training techniques is estimated,
operating room training is far more expensive and the
transfer effectiveness of simulation training is more than
twice that of box or actual operating room experience. A
competency based curriculum accounts for differences
in ability and skill at the outset, eliminates the learning
curve in the operating room, and pre-trained residents
learn much more effectively when they do enter the
operating room. It also ensures that basic competencies
are achieved and tested. The essential components of
a successful curriculum based on American College of
Surgeons consensus meetings (1) include development of
cognitive, psychomotor and team skills. The animal lab
serves as the final testing ground before the operating
room. Team training has been largely ignored in surgical
education and there is a need for educational interventions
in this domain (currently only half of the Canadian
and 30% of the US programs offer team training component).
Figure 1 illustrates the essential elements of
team training: situation awareness, leadership, teamwork
and decision making.
|
Teodor told us that error is inevitable if humans are
involved and the "deny, forget, ignore and repeat" response
is unacceptable. The solution is performance analysis, education,
and deliberate practice to mitigate errors and interrupt
the chain of events that leads to adverse outcomes (Fig.
2). Teodor's group has developed a black box multichannel
performance analyzer to reduce surgical errors. It records
many variables in the operating room, including noise and
distractions. The pathway for interrupting this is analysis,
identification, awareness, early detection.
Vanessa Palter, working with Teodor, reported a
randomized control trial in the Annals of Surgery, comparing
conventionally trained with competency-based
curriculum trained surgical residents. The difference was
striking (Fig. 3).
In the discussion period, Jim Rutka asked about the
problem of taking uncorrectably non-proficient surgeons
all the way through training. Teodor answered that 5%
of residents show outstanding abilities at the outset, 8%
never become proficient and the rest achieve proficiency
with training. Training individuals who don't have the
innate abilities is a waste of personal and training-system
resources. To find a way to screen out those who should
not become surgeons, Teodor is working with medical
student volunteers, using functional MRI to determine
aptitude or ineptitude.
M.M.
(1) Zevin B, Levy JS, Satava RM, Grantcharov TP. A Consensus-Based Framework for Design, Validation, and Implementation of Simulation-Based Training Curricula in Surgery. Journal of the American College of Surgeons: October 2012: 215 (4): pp 580-586.e3
|